Newsletter

Prenatal ultrasonographic approach to skeletal dysplasia: Practical tips
What is the ideal time to look for the skeletal dysplasia?
The long bones, vertebrae and calvarium begin ossifying by 12 weeks, so the presence of certain skeletal dysplasias especially the lethal ones can be suggested as early as the first trimester.
When should we suspect for skeletal dysplasia?
Any fetus showing femoral length (FL) or humerus length (HL) measurements less than 5th centile or −2 SD from the mean at all gestations should be evaluated.
Table 1: Checklist to approach to the skeletal dysplasias.
| Gestational age based on LMP or first trimesterultrasound (IUGR/Constitutional) |
| Long bones-Absence/Length (femurs, humerus, radius, ulna, tibia, fibula,and clavicle) |
| Shape (straight, curved, bilateral vsunilateral) |
| Appearance of the metaphyseal ends (spikes, irregularities) |
| Echo density(well mineralized, poorly mineralized) |
| Foot (size and shape) |
| Hands (poly/syn/oligo – dactyly, trident hand, talipes, hitchhikers thumb/toe) |
| Circumferences (head, abdomen, and chest) |
| Skull (mineralization, suture, shape like cloverleaf, size) |
| Thorax (champagne cork shape, barrel shaped, bell shaped) |
| Ribs (short, fracture/beaded, absent/disorganised) |
| Scapula (size and shape) |
| Presence of the secondary epiphyses (calcaneus >20 wk, kneeepiphyses >28 wk) |
| Mandibular size and shape |
| Fetal profile (frontal bossing, absent/flat nasal bone, micrognathia, cleft lip/palate, orbits) |
| Vertebral bodies (Mineralization, hemivertebrae,disorganised and shape) |
| Other congenital anomalies (CNS, cardiac, renal, anterior abdominal wall, genitals) Evaluation of amniotic fluid volume (hydramnios) Hydrops |
Table 2:Important ratios to evaluate skeletal dysplasia.
| Biometric ratios | Findings | Interpretation | |
|---|---|---|---|
| 1 | Short femur (FL) | >4 SD below the mean | Lethal(8) |
| Short femur (FL) | < 4 SD below the mean | Suggestive of a skeletal dysplasia. | |
| 2 | FL: footlength | <1 | Suggestive of a skeletal dysplasia(9). |
| 3 | 3D USG lung volume | ≥5th percentile for gestational age | Non-lethal |
| 3D USG lung volume | <5th percentile for gestational age | Lethal(10). | |
| 4 | FL:AC | <0.16 | lethal (With polyhydramnios mostly lethal) |
| FL:AC | >0.16 | Non-lethal(11). | |
| 5 | CC:AC | <0.6 | Lethal |
| CC:AC | <0.6 | Non-lethal(12). | |
| CC:AC | <0.6 | Non-lethal(12). |
- The femur length is more than >5 mm below 2 standard deviations (equivalent to greater than 4 standard deviations below the mean), the sonologist can be certain he or she is dealing with a significant skeletal dysplasia (Fig. 1a) (8). Femur length normalized chart is in Table
- The femur/foot length ratio (FL: foot) nomogram appears to be a useful parameter to help differentiate fetuses that have dysplastic limb reduction from those whose limbs are short because of constitutional factors or IUGR, significant correlation was demonstrated (r = 0.98; P less than .0001) (Fig. 1b)(9).
- 3D US calculated lung volumes compared to normal fetuses (
- Femur length to abdominal circumference ratio (FL:AC), (Sensitivity 92–96%) whencombined with the presenceof polyhydramnios, the ability to predict lethality has been reported tobe as high as 100% (11) (Fig. 1c).
- Chest circumference to abdominal circumference ratio (CC:AC), chest circumference to abdominal circumference ratio had the highest diagnostic accuracy for antenatal diagnosis of pulmonary hypoplasia (sensitivity: 93.5% and specificity: 90.3%) independent of gestational age (Fig. 1d) (12).
Lethality occurs in most skeletal dysplasia’s as a result of a small chest circumference and resultant pulmonary hypoplasia(13).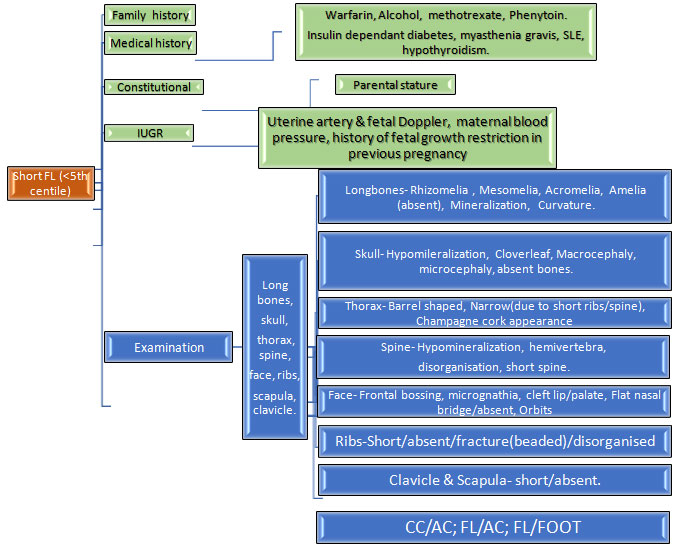 Flowchart 1.Systematic approach to evaluate
Flowchart 1.Systematic approach to evaluate
Table 3: Ultrasound findings in Major skeletal dysplasias’s:
| Diagnosis | Skeletal system – Femoral length (FL) is <5th centile PLUS | Other systems | |
|---|---|---|---|
| 1 | Achondrogenesis 1 | Limbs: severe shortening;Trunk: shortHead: macrocephaly with frontal bossingThorax: NarrowSkull: hypo-mineralisationSpine (vertebral bodies): Hypo-mineralisationThorax: rib fractures |
|
| 2 | Achondrogenesis2 | Limbs: severe shortening;Trunk: shortHead: macrocephaly with frontal bossingThorax: NarrowSkull: hypo-mineralisationSpine (vertebral bodies): no/minimal Hypo-mineralisationThorax: no ribfractures |
|
| 3 | Achondroplasia | Limb: short (>22 weeks), trident hands (Fig. 2a)Head: macrocephaly with frontal bossing (Fig. 2b)Spine: lumbar lordosis.Thorax: normal |
|
| 4 | Campomelic dysplasia | Limb: short, bowed legs, arms normal length, club feet.Thorax: narrowScapulae: hypoplasticHead: large with small faceAmbiguous genitalia +/- | |
| 5 | Cleidocranial dysplasia | Limb: shortSpine (vertebral bodies): poor mineralizationSkull: mild hypomineralizationClavicle: hypoplastic | |
| 6 | Conradi-hunermann- Happle syndromeLimb: rhizomelic shortening, stippled epiphysis Spine: stippledThorax and skull: normal |
Cataract, midface hypoplasia | |
| 7 | Rhizomelic Chondrodysplasia punctata |
Limb: rhizomelic severe shortening Stippled epiphyses (Fig. 2c)Head: late onset microcephaly Skull & thorax: normal.Others: nasal hypoplasia (Fig. 2d, 2e), cataract. |
|
| 8 | X-linked recessive Chondrodysplasia punctata |
Limb: shortening with stippled EpiphysesThorax: normalSkull: normalOthers: larynx and sternum Stippled epiphyses,Face: nasal and distal phalangeal hypoplasia |
|
| 9 | Diastrophic dysplasia | Limb: very short & bowing,Joints: flexion contracture, talipesOthers: hitchhiker thumb/toeSpine: scoliosisThorax: normalSkull: normal | |
| 10 | Ellis van Creveld Syndrome |
Limb: acromelic&mesomelic shorteningPostaxial polydactylyThorax: smallSkull/spine – normal. | Cardiac anomaly- ASD >50% Posterior fossa cyst |
| 11 | Hypophosphatasia- severe neonatal form | Limb: very short, acute angulationThorax: small narrow with short ribsOther: hypomineralization of all long bones, skull, ribs, vertebrae, talipes |
Polyhydramnios |
| 12 | Hypophosphatasia- variable onset | Limb: very short, acute angulation (decreases with gestation)Thorax: small narrow with short ribsOther: hypomineralization all long bones, skull, ribs, vertebrae, talipes | |
| 13 | Juenes asphyxiating thoracic dystrophy | Limb: short, 22weeks, polydactyly Thorax: narrow (Fig. 2f) and short ribs Skull spine: normal |
Renal anomalies |
| 14 | Osteogenesis imperfecta IIA/C | Limb: short with fracturesThorax: small with fractured ribsSkull: hypomineralization. | |
| 15 | Osteogeneis imperfecta IIB/III/IV | Limb: mild shortening & bowed long bonesSkull: mild hypomineralizationThorax: normal/slightly smallSpine: scoliosis |
|
| 16 | Osteogenesis imperfecta VIII | Limb: very short <3rd centile with bowed long bonesSkull: mild hypomineralizationThorax: normal/slightly small with fractured ribs |
|
| 17 | Roberts syndrome | Limb: short/absent Oligodactyly, talipes,Skull: normalThorax: normal |
Cardiac anomalies, cleft lip/palate. |
| 18 | Thanatrophic dysplasia type I | Limb: very short, trident handThorax: narrow with short ribsTrunk: normalSpine: Platyspondyly (type I>II).Head: macrocephaly with frontal bossingFemur: curved or bowing of femur (telephone receiver) (Fig. 2g). | Polyhydramnios- 50% |
| 19 | Thanatrophic dysplasia type II | Limb: very short, trident handThorax: narrow with short ribsTrunk: normalSpine: Platyspondyly (type I>II).Head: macrocephaly with frontal bossingFemur: straightSkull: cloverleaf- shaped | |
| 20 | Spondylo-epiphyseal-dyplasia congenita | Limb: shortThorax: short with normal ribsSkull: normalSpine: hypomineralised vertebral bodies | |
| 21 | Short-ribbed polydactyly syndromes I (Saldino-noonan) | Limb: severe micromelia (<<3rd) Polydactyly Thorax: smallSkull: normal |
Generalized skin oedema |
| 22 | Short-ribbed polydactyly syndromes II (Majewski) |
Limb: severe shortening, polydactylyThorax: small with short ribSkull: cloverleaf (Fig. 2h)Others: exomphalos, bladder outflow obstruction, midline facial cleft |
Generalised skin odema, CNS anomalies. |
| 23 | Short-ribbed polydactyly syndromes III (Verma-Naumoff ) |
Limb: normal <10th centile, Postaxial polydatyly Thorax: small Skull: normal |
What is the role of 3D USG?
The overall accuracy for the diagnosis of the specific type of skeletal dysplasia using routine USG approaches only 40%-60%,which can be enhanced by the use of other imaging modalities. 3dimentional USG is helpful in differentiating the fetal facial abnormalities and in the evaluation of fetal limbs better, for example: severe flattening of the nasal bridge and craniosynostoses in thanatophoric dysplasia. Fetal MRI has been reserved for cases with suspected spinal abnormalities in the form of scoliosis or diastemetomylia. (14)
Is there any role for MRI in the diagnosis of skeletal dysplasia?
MRI has superior soft tissue contrast, better resolution, ability to examine both sides of the fetus simultaneously and also provide information about the stages of maturation of gray and white matter. Similar to USG it does not expose the fetus to ionizing radiation and has no teratogenic effect during pregnancy. (15) Echoplanar MRI may also be valuable in determining the presence or absence of ossification. Skeletal dysplasias such as osteogenesis imperfecta and hypophosphatasia, present with a generalized decrease in osseous density, which is demonstrated as lack of hypointense signal (indicative of normal ossification) on echoplanar imaging sequences. (16)
Prenatal use of CT scan in the diagnosis?
In a study conducted by Miyoko et al 3D-CT was more accurate than was 2D ultrasound in visualizing vertebral anomalies (abnormal shape of the vertebral bodies, abnormal interpedicular distance), pelvic bone malformations (delayed ossification of the pubic bones, abnormal acetabular shape) and enlarged metaphysis or synostoses in long bones. Both imaging techniques are useful in the management of fetal dysplasia; 2D ultrasound is a useful screening test and 3D-CT is a valuable complementary diagnostic tool (14). Because of the associated radiation dose, which may be similar to that of conventional fetal radiography, the use and potential impact of CT is limited. (17). There are ongoing newer studies on low dose 3D CT, where the dose is below 100mGy, reducing the overall exposure risk to mother and fetus.
What investigations are recommended in women who opt to discontinue the pregnancy?
Cases of suspected lethal skeletal dysplasia where the couple opt to discontinue the pregnancy or where there has been an antepartum stillbirth ,in order to reach a specific diagnosis a minimum post-delivery work up should include(a)external examination with photographs anterior and posterior of the appendicular and axial skeleton including hands and feet(b)post whole body radiographs/infantogram anteroposterior and lateral views (c)skin or tissue biopsy specimens for chromosome analysis or preservation of fibroblasts/DNA storage (d)if possible a complete autopsy should be performed. (18)
How to counsel the couple?
In cases where there is a previous molecular diagnosis of a childaffected by skeletal dysplasia, there is a role of prenatal diagnosis in the form of chorionic villous sampling or amniocentesis.In situations where either of the parent has a clinically identifiable skeletal dysplasia, they should be encouraged to get a molecular diagnosis before planning pregnancy.Role of Non-invasive testing in the diagnosis of Skeletal Dysplasia
There are several studies about the different techniques used for the non-invasive prenatal testing (NIPT) of achondroplasia like conventional PCR with restriction enzymes, matrix assisted laser desorption/ionization(MALDI) time of flight mass spectrometry, real time quantitative PCR, digital PCR and next generation sequencing (19-23).In 2019 Vivanti etal (24) reported the results of a novel simple non-invasive molecular analysis technique using high-resolution melting (HRM) analysis for the prenatal diagnosis of achondroplasia in a prospective multicentre cohort study. They also suggested thatcell free DNA can be advised in the first trimester in cases where there is history of an affected child with FGFR3 related skeletal dysplasia or where the father is affected but for technical reasons it cannot be applied to pregnant women who are affected by the disease, as their plasma contains a background of mutated DNA. NIPT can also be offered where neither of the parent is affected but FGFR3 related skeletal dysplasia is suspected in the fetus on the basis of USG.
How do we manage the pregnancy and labour?
The aim of antepartum care is to reach a final diagnosis as to the type of skeletal dysplasia the baby has, as that is one of the main indicators of the final outcome. The delivery should be planned in a tertiary care centre with a multidisciplinary team consisting ofan obstetrician,neonatologist, paediatric orthopedician and emergency medicine specialist. If possible, instrumentation during delivery should be avoided when fetal skeletal dysplasia is suspected due to the increased risk of intracranial and cervical spine complications.(25)Caesarean section is usually performed for obstetric indications or in cases where the biparietal diameter (BPD)>40cm.The role of elective caesarean section in women carrying a baby with suspected Osteogenesis imperfecta is controversial with newer guidelines indicating that an elective caesarean section vs a vaginal delivery does not reduce the risk of fractures(26). Postnatal genetic evaluation should be performed in order to confirm the diagnosis and also to assess the recurrence risk in future pregnancies.
References:
- Barbosa-Buck CO, Orioli IM, da Graça Dutra M, Lopez-Camelo J, Castilla EE,Cavalcanti DP. Clinical epidemiology of skeletal dysplasias in South America. AmJ Med Genet A 2012.
- Geert R. Mortier,Daniel H. Cohn,et al, Nosology and classification of genetic skeletal disorders: 2019 revision, Am J Med Genet. 2019.
- Parilla BV, Leeth EA, KambichMP et al (2003) Antenatal detection of skeletal dysplasias. J Ultrasound Med.
- Gaffney G,Manning N, Boyd PA et al (1998) Prenatal sonographic diagnosis of skeletal dysplasias–a report of the diagnostic and prognostic accuracy in 35 cases. Prenat Diagn.
Join Us

Become a FMF India Member
Get information on
- Upcoming events
- Information on seminal papers published in fetal medicine
- Regular free webinars on new development in the field of fetal medicine
- Be part of a community where collaboration and interaction will be possible with other like minded people
Contact Us
Questions or Comments? Contact us and we'll get right back to you.
Fetal Medicine Foundation - India 13, Babar Lane, New Delhi - 110001
Tel: +(91) - 11 - 71793018 +(91) - 11- 26925858, Extn. 3018
Join Us
Become a member to get information on upcoming events, seminal papers published in fetal medicine, regular free webinars, and to collaborate and interact with like minded community.
Fetal Medicine Foundation India. Registration Number S/109/2012 under Societies Registration Act, 1860
- About
- | Courses & Programmes
- | Events & Seminars
- | Blog
- | Privacy Policy
- | Terms & Conditions
- | Contact Us
- About
- Courses & Programmes
- Events & Seminars
- Blog
- Contact Us
- Privacy Policy
- Terms & Conditions
Copyright@FMFIndia.in 2024

