Introduction: Skeletal dysplasia are a heterogenous group of disorders which affect the natural development of skeletal system and manifest as abnormalities of limbs, chest, skull or spine. These are genetic diseases which result in abnormal formation of chondro-osseous tissues. Their prevalence varies from 1:5000 to 1:3000 births with such wide variation primarily because of incomplete evaluation of still births and early neonatal deaths in several studies (1). These disorders contribute to a significant proportion of still births and early neonatal deaths, however several of them have better prognosis with survival well into adulthood. They have a varied clinical presentation and can be diagnosed at various ages due to this variable presentation (2). A comprehensive knowledge of these disorders is required for timely suspicion, complete examination, appropriate testing and diagnosis. Early and correct diagnosis is essential as most of these cases are lethal and a diagnosis helps in subsequent pregnancies.
Clinical presentation: Skeletal dysplasias may present in either of the following four presentations: (I) Still birth with antenatal suspicion (growth retardation, short bones, vertebral and facial anomalies) with/without antenatal diagnosis (II) still birth undiagnosed with postnatal findings of shorening, limb, chest or facial anomalies (III) neonate with shortening of trunk and/or limbs, facial anomalies, respiratory insufficiency, fractures (IV) infancy to adulthood with short stature and limb or spine deformities, fractures, eye/ear/dental abnormalities.
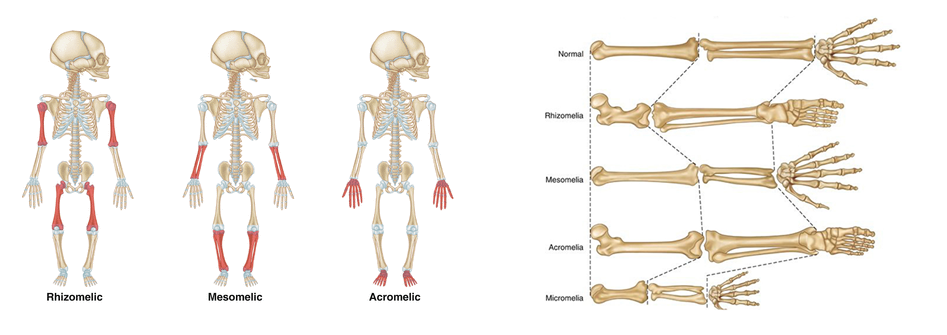
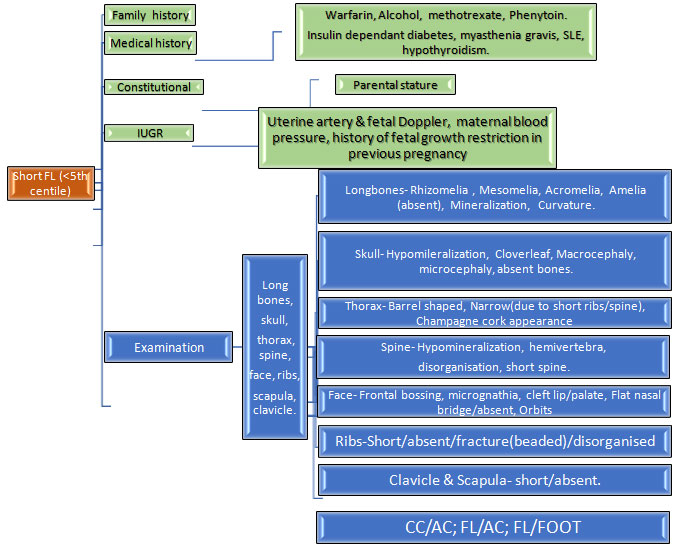
Clinical evaluation of a case of suspected skeletal dysplasia: Skeletel dysplasia is a very broad group involving host of disorders. The ones which present during neonatal period are listed in table 1 along with their features. A complete head to toe examination is required to find out all the abnormalities which can help in diagnosis. Skull should be examined for shape (barchycephaly, clover leaf, craniosynostosis), facial abnormal features like hypo/hypertelorism, cleft lip/palate, dentition anomalies, thorax should be examined for size, signs of respiratory insufficiency, spine should examined for kyphoscoliosis, limbs examined for shortening and contractures, site of shortening like proximal (rhizomelia), middle (mesomelia), distal (acromelia). Femur length-foot length ration less than 1 suggests skeletal dysplasia. Table 2 illustrates these clinical features along with their associated causes.
Radiological evaluation of a case of suspected skeletal dysplasia: A comprehensive and detailed skeletal survey is essential in aiding in diagnoses (3,4). Survey must include AP & lateral views of skull and thoracolumbar spine, AP views of chest, pelvis, one upper and lower limb, left hand (for bone age). The axial and appendicular skeleton must be properly examined for abnormalities like workman bones, thick skull, degree of ossification, platyspondyly (flat vertebral body), coronal clefts (radiolucent band running through at least one vertebral body), abnormal vertebral bodies like central beaking in Morquio’s disease and posterior hump shaped in SEDT. In appendicular skeleton, the site of affection (epiphyses, metaphases or diaphyses), type of limb shortening (rhizomelia, mesomelia, acromelia). The aetiologies associated with these findings are elaborated in table 2.
Postnatal management: After the delivery of a case of suspected skeletal dysplasia, initial stabilisation is very crucial which is to be followed by multi-disciplinary approach to diagnosis and ongoing care. Table 3 depicts the summarised care of such a baby. It is very essential to obtain samples for genetic tests for diagnosis as many of these disorders have poor prognosis and antenatal diagnosis in future pregnancies is crucial.
Conclusion: Skeletal dysplasia is a group of disorders with varied presentation and a strong clinical suspicion is necessary for timely diagnosis as outcomes are not very good. A multidisciplinary team approach is necessary to ensure a proper quality of life to survivors. Appropriate timely antenatal diagnosis at this point is primarily the mode of management. Future research on gene therapy and other treatments are required for ensuring better survival and quality of life to these individuals.
| Category | Disease name | Clinical and radiologic features | Genes involved, inheritance and prognosis |
|---|---|---|---|
| FGFR3 group | Thanatropic dysplasia |
|
|
| Achondroplasia |
|
|
|
| Hypochondroplasia | Similar to achondroplasia, milder severity, later onset in second decade |
|
|
| Type II collagen group | Achondrogenesis type II |
|
|
| Hypochondrogenesis |
|
|
|
| Kniest dysplasia |
|
|
|
| Spondyloepiphyseal dysplasia congenita |
|
|
|
| Stickler syndrome |
|
|
|
| Short rib dysplasia group | Ellis van Crevald syndrome |
|
|
| Asphyxiating thoracic dysplasia (Jeune) |
|
|
|
| Decreased bone density group | Osteogenesis imperfecta type I-IX |
|
|
| Defective mineralization group | Hypophosphatasia
|
|
|
Table 1: Skeletal dysplasia which present during neonatal period. Abbreviations: AD autosomal dominant, AR autosomal recessive.
| Part of body | Clinical or radiological feature | Possible ethology |
|---|---|---|
| SKULL | Macrocephaly/ Microcephaly | TD, achondroplasia, JLS/ CDP |
| Irregular skull shape | TD (cloverleaf), CDP, JLS | |
| Hydrocephalus | CD, Oi type 2, osteoporosis | |
Normal size
|
CCD, OI type 1 & 2CCD
CCD, OI type 2, achondrogenesis |
|
| Wormian bones/ Thick skull | CCD, PD, OI, hypophosphatasia, Osteopetrosis, CFD | |
| FACE | Facial anomalies (micrognathia, hypo/hypertelorism, frontal bossing | CDP, achondroplasia, CD, cleidocranial dysplasia, DD, OI type 1, SEDC |
| Cleft lip or palate/ Gingival frenulae | SRPS, CD/EVS | |
Eye abnormalities:
|
CCD/CDP | |
Teeth
|
EVSCCDOIHypophosphatasia | |
| THORAX | Narrow
|
Osteopetrosis, CCD, EVSTD, CCD, JLSOI type 1&3TD, achondrogenesis, OI type 3 |
| Short barrel shaped | JLS, SEDC | |
| LIMBS | Normal limb echogenecity with severe shortening
|
Amelia, osteoporosis, SRPS, CCD, EVS TD, CCD, JLS OI type 1&3 TD, achondrogenesis 1A & 1B, OI type 3 HC, JLS, OI type 3, SRPS, SEDC DD, FHUFS |
Normal limb echogenecity with mild to moderate shortening
|
EVSMesomelic dysplasia, SEDCOI type 1, SRPS, SEDC | |
Decreased limb bone echogeenicity
|
Achondrogenesis, OI type 1 & 2 OI type 2 |
|
| Hypoplastic nails | EVS, CDP | |
| SPINE | Platyspondyly | MD, Morquio syndrome, OI, TD, KD |
| Coronal cleft | CDP, MD, KD |
Table 2: Clinical features in case of skeletal dysplasia. Abbreviations: OI osteogenesis imperfecta, TD thanatropic dysplasia, JLS Jarcho-Levin syndrome, CDP chondrodysplasia punctata, CD campomelic dysplasia, CCD cleidocranial dysplasia, CDP chondrodysplasia punctata, DD diastrophic dysplasia, SEDC spondyloepiphyseal dysplasia congenita, SRPS short rib polydactyly syndrome, EVS Ellis van Creveld syndrome, HC Hypochondroplasia, FHUFS femoral hypoplasia-unusual face syndrome, MD metatrophic dysplasia, KD Kniest dysplasia, CFD craniofacial fibrous dysplasia, PD pyknodysostosis
| Arm of treatment | Components |
|---|---|
| Initial stabilisation | Airway and breathing:
Circulation:
Neurological: Seizures management with AED
Others: Handling: if suspicion of OI then gentle handling and supportive care to prevent fractures
|
| Multidisciplinary approach to diagnosis |
|
| Specific therapies |
|
| Postmortem analysis | Include the following:
|
Table 3: Postnatal management in case of suspected skeletal dysplasia. Abbreviations: BP blood pressure, CFT capillary refill time, PPHN persistent pulmonary hypertension, OI osteogenesis imperfecta, CKD chronic kidney disease.
References:
- Andreas Zankl.Genetics of Bone Biology and Skeletal Disease (Second Edition), 2018
- Seth J Langston, Deborah Krakow, Alison Chu. Revisiting Skeletal Dysplasias in the Newborn. Neoreviews 2021 Apr;22(4):e216-e229.
- G R Mortier. The diagnosis of skeletal dysplasias: a multidisciplinary approach. Eur J Radiol 2001 Dec;40(3):161-7.
- D Krakow. Skeletal Dysplasias. Clin Perinatol. 2015 June ; 42(2): 301–319.